Varicocele
What is a varicocele?
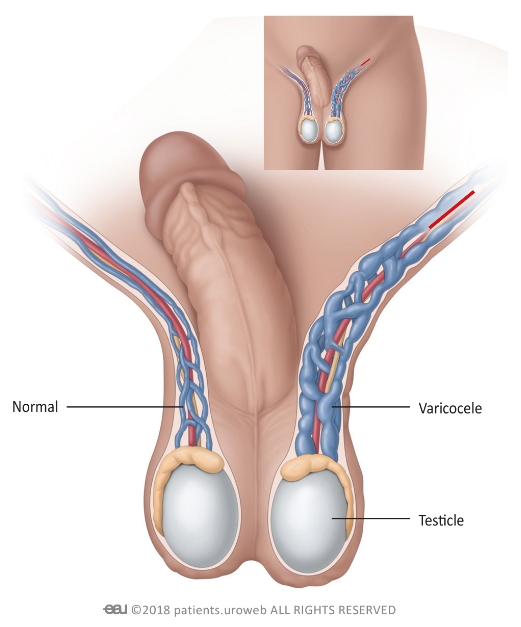
A varicocele (vary-ko-seel) is a mass of enlarged veins which develops in the scrotum, similar to varicose veins which occur in the legs. About 15% of men develop them during puberty and they disproportionately affect the left side of the scrotum. They often do not cause any complications, though some can decrease sperm movement and impact fertility.
Sandhurst Urology offers diagnosis, management, and medical interventions for varicoceles from our clinic in Bendigo. To book an appointment, please ask your GP for a referral.
Symptoms of a varicocele
Most varicoceles do not cause day-to-day symptoms, and around eight out of ten men who have them will not experience negative impacts on their fertility.
If your varicocele produces symptoms, they may include:
- A dull, aching pain in the scrotum
- Recurring scrotal pain
- One testicle appearing smaller than the other (particularly on the side with the varicocele)
- Infertility and decreased sperm count
- A painless lump on or above one testicle
- Large, twisted veins on the scrotum (often described as looking like a bag of worms)
- Swelling or a bulge in the scrotum
Remember that your own experience with varicoceles is individual – you may not experience every symptom and may experience slightly different symptoms to those specified. For further advice and diagnosis, book an appointment at Sandhurst Urology.
How varicoceles are diagnosed
Your doctor usually begins diagnosing a varicocele with a physical exam. They will visually inspect the testicles and scrotum, feel for abnormal shapes or growths, and ask about your medical history. Because varicoceles are not always easy to see or feel, your doctor may ask you to alternate between standing and sitting during the exam so they perform a more thorough assessment.
If your doctor suspects a varicocele, they may request further tests to conform it and assess it in detail. These tests may include:
- Valsalva manoeuvre – your doctor may ask you to stand up, take a deep breath, hold it, and bear down with your abdominal muscles as they examine the scrotum. This increases the pressure inside your abdomen, making a varicocele easier to identify if present. The Valsalva manoeuvre is sometimes combined with an ultrasound to see how blood moves through the varicocele.
- Ultrasound – using sound waves to create an image of the body’s soft structures, this test can let a doctor identify varicoceles and assess their severity. Your doctor may also request an ultrasound of the kidneys to check for small tumours which sometimes occur alongside varicoceles in older men.
- Semen testing – though it does not diagnose the varicocele itself, your doctor may recommend analysing your semen and sperm to assess the varicocele’s impact on your fertility. The information it provides can help assess the varicocele’s severity and inform your treatment.
- Blood tests – though they do not diagnose a varicocele directly, blood tests can help rule out other causes for your symptoms. Your doctor may request them to rule out other causes of infertility.
Preventing varicoceles
There are currently no medications, activities, or lifestyle factors that are known to directly prevent varicoceles from forming. However, maintaining a healthy lifestyle can improve your circulatory health and may therefore reduce venous anomalies such as varicoceles. In addition to any recommended by your medical team, strategies to do this may include:
- Caring for your kidneys – kidney tumours can block blood flow and cause a varicocele to develop. If you are at risk of developing renal cancers (particularly if you are over 50), regular health checks and monitoring may help catch both them and varicoceles in their early stages.
- Avoiding smoking – tobacco consumption can affect the structure and function of blood vessels, making them more prone to plaque build-up and malformations. Refraining from tobacco consumption may therefore decrease your risk of developing the faulty blood vessels which characterise a varicocele.
- Staying physically active – regular exercise promotes healthy blood flow and improves circulation, which may reduce your chances of developing a varicocele.
As with any condition, always seek medical guidance to prevent and treat varicoceles effectively. Ask your GP for a referral to Sandhurst Urology for individualised advice.

Treatments for varicoceles
Non-surgical treatments can include:
- Pain medications – over-the-counter painkillers such as Panadol or Nurofen do not treat varicoceles directly, though they can reduce pain levels and make living with them easier.
- Using a scrotal support – wearing a jockstrap, athletic supporter, or tight brief underwear can help manage pain levels.
- Considering fertility treatments – if your varicocele impacts your fertility, you may wish to consider other treatments which increase your likelihood of having a child. These may include hormone therapy or using a sperm donor.
- Manage kidney tumours – varicoceles are sometimes caused by kidney tumours which block blood flow through a vein. Treating the kidney tumour may restore blood flow and reduce the varicocele’s appearance as a result.
Medical interventions for varicoceles
Sandhurst Urology offers a suite of medical and surgical procedures to treat varicoceles in Bendigo. Options include:
- Varicocelectomy – this short surgery involves the doctor physically removing the enlarged veins by cutting them and tying them off. A varicocelectomy can often be performed laparoscopically, resulting in only one or two small scars on the lower abdomen after healing.
- Varicocele embolization – The surgeon can pass a thin catheter into the vein through a small incision, then use it to place small coils inside the enlarged vein. This reduces or blocks blood flow through the varicocele which can cause the blood vessels to shrink.
Providing Excellent Urological Care of the Highest Standards
Book a consultation with Sandhurst Urology today