Bladder tumours
What are bladder tumours?
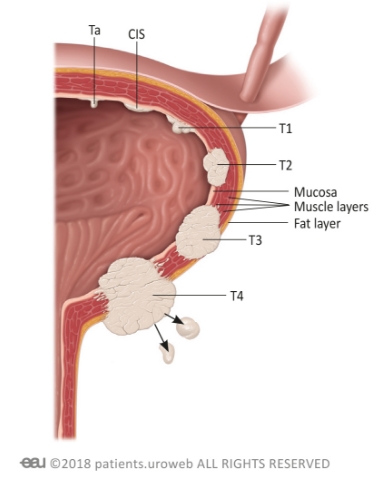
Bladder tumours are one of the most common cancers affecting Australians. The most common variety of bladder tumour is urothelial carcinoma, beginning in the bladder wall’s innermost layer and sometimes spreading into nearby structures. Bladder tumours may be accompanied by ureteric tumours, both of which are related to exposure to certain chemicals, and therefore have a higher risk of occurrence later in life.
Sandhurst Urology offers diagnosis, management, and medical intervention for bladder tumours from our clinic in Bendigo. To book an appointment, please ask your GP for a referral or call us directly.
Symptoms of bladder tumours
Many bladder tumours do not produce noticeable symptoms in their early stages. As the tumour progresses and begins to impede regular functions, patients with bladder tumours may experience:
• Blood in the urine
• Pain when urinating (often a burning sensation)
• Frequent urination
• Difficulty urinating
• Lower back pain
• Tiredness or weakness
Remember that your own experience with bladder tumours is individual – you may not experience every symptom and may experience slightly different symptoms to those specified. For further advice and diagnosis, book an appointment at Sandhurst Urology.
How bladder tumours are diagnosed?
Bladder tumours are generally diagnosed with the results of multiple tests. If you exhibit symptoms of a bladder tumour, your doctor may request some of the following tests:
- Cystoscopy – a minimally invasive procedure which allows your doctor to see inside the bladder. Under a local anaesthetic or light sedation, a urologist passes a tiny camera through your urethra and into your bladder. This allows them to visually inspect potential tumours.
- Urine cytology – you may be asked to provide a small urine sample in a cup, which will be sent to a pathology lab where it is analysed for cancer cells. This shouldn’t be the first void of the day, and may e required to e performed up to 3 times for that assessment.
- Bladder biopsy – this involves removing a small amount of bladder tissue, which is analysed in a pathology lab for cancer cells. In most cases, your urologist will take the sample during a cystoscopy.
- CT urogram – a test which combines injectable dye and targeted x-rays to get a clear image of your urinary system, helping your urologist assess the size and shape of your bladder. They may also assess the kidneys and ureters at the same time.
Further imaging and tests may also be used to assess whether the bladder tumour has spread to other parts of the body.
Preventing bladder tumours
While it is not possible to completely prevent bladder cancer, there are some steps you can take to reduce your likelihood of developing it. In addition to specific advice provided by your medical team, the following strategies may help:
- Manage chemical exposure – some chemicals used in manufacturing dyes paints, rubber, leather, and textiles have been linked to bladder cancer. If you work in an environment with these chemicals, take care to limit your exposure.
- Avoid smoking – smoking tobacco is a risk factor for most types of cancer. As the body excretes many of tobacco’s harmful chemicals through the urine, it is particularly likely to harm your bladder.
- Adopt a healthy diet – some studies suggest that the antioxidants found in vegetables such as broccoli, cabbage, and kale may decrease your risk of developing bladder tumours.
As with any condition, always seek medical guidance to prevent and treat bladder tumours effectively. Ask your GP for a referral to Sandhurst Urology for individualised advice.

Treatments for bladder tumours
Your treatment options for bladder tumours will vary depending on the size of your tumour, its type, whether it has spread to other parts of your body, and your overall health. Your available nonsurgical treatment options may include:
- Chemotherapy – strong medications which use powerful chemicals to kill cancer’s fast-growing cells. They may be administered intravenously, or through a catheter directly into your bladder.
• Radiation therapy – using targeted radiation like x-rays, gamma rays, or proton beams, this treatment can destroy the bladder tumour’ cells while minimising harm to healthy cells. It is often used alongside other bladder cancer treatments. - Targeted therapies ¬– these medications act on the cancer’s specific genes, proteins, or tissue environment to stop it from growing. Targeted therapy treatments can be very individualised and are often offered in conjunction with other therapies.
- Immunotherapy – Bacillus Calmette-Guerin (BCG) can be administered into the bladder to prompt your immune system to attack foreign proteins such as cancer cells. Your urologist will guide you on this form of treatment.
- Lifestyle modifications – while they will not actively fight your tumour, altering the way you live may help reduce symptoms.
Medical Interventions for bladder tumours
Many bladder tumours require surgery to remove completely. If operative treatments are needed, your surgeon will discuss all available options and help decide on which will be most effective. Treatments offered through Sandhurst Urology’s Bendigo clinic include:
- Tumour removal – Some tumours can be cut away from the bladder without significantly damaging it. Sandhurst Urology can provide this service using endoscopic techniques, removing the tumour through your urethra with no external incisions needed.
- Cystectomy – Muscle invasive bladder cancer is a very aggressive disease and needs to be managed accordingly. If the tumour has spread deep into the tissue, your best treatment option may be to remove the bladder entirely (cystectomy). As a cystectomy can radically alter how the urinary system works, your surgeon will also speak to you about your options for managing urine afterward.
- Bladder reconstruction – if your bladder tumour treatment requires removing your whole bladder, your urologist may use a section of your intestinal tract to construct a pouch in your abdomen. The new pouch, called a neobladder, holds urine and allows you to pass it as normal. This is not suitable for all patients and your urologist will guide you on this.
- Urinary diversion – treating a bladder tumour may require creating a new passage for urine to exit your body. The passage may be temporary, letting the bladder rest as it recovers from another procedure, or a permanent pathway which requires periodic draining.

Providing Excellent Urological Care of the Highest Standards
Book a consultation with Sandhurst Urology today