Testicular cancer
What is testicular cancer?
Although uncommon, testicular cancer is the second most diagnosed cancer in young Australian men. Fortunately, testicular cancer is very treatable and over 97% of people diagnosed survive for at least 5 years afterwards.
There are two main types of testicular cancer: seminomas and non-seminomas. Seminomas are slow-growing and generally affect men in their 40s or 50s, while non-seminoma cancers are more common in younger men aged between their late teens and early 30s. Some testicular cancers contain both seminoma and non-seminoma cells.
Sandhurst Urology offers diagnosis, management, and medical intervention for testicular cancer from our clinic in Bendigo. To book an appointment, please ask your GP for a referral.
Symptoms of testicular cancer
Most testicular cancers do not cause pain or swelling, though most result in a solid-feeling lump inside the scrotum. In addition to this, symptoms may include:
- Pain or discomfort in the scrotum
- Pain or discomfort in one or both testicles
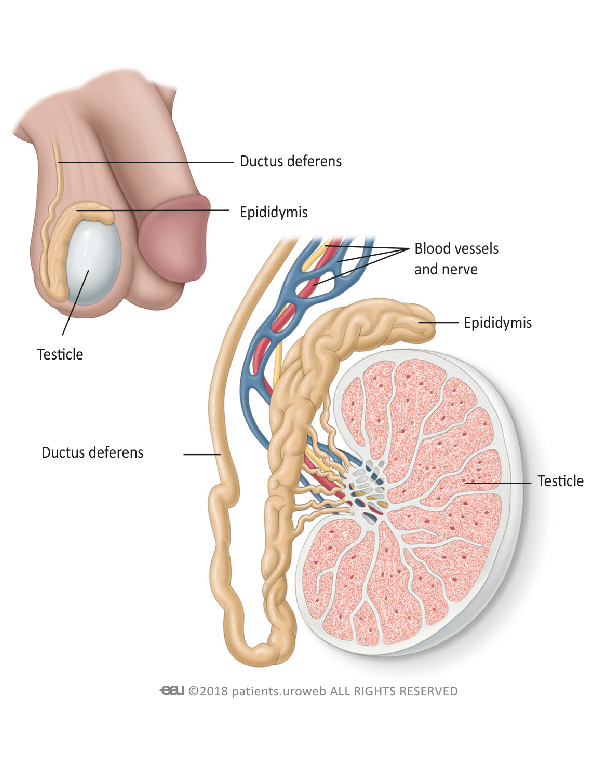
- Feeling a painless lump in either testicle or in the epididymis (the tube at the back of the testicle)
- Swelling or enlargement in one or both testicles (with or without pain)
- A heavy feeling in the scrotum
- One testicle feeling firmer than the other
- The testicles feeling uneven
- A dull ache in the back and/or lower abdomen
- Dull aches or pains in the scrotum or groin
- Enlarged or tender breast tissue
- Fluid collecting in the scrotum
Remember that your own experience with testicular cancer is individual – you may not experience every symptom and may experience slightly different symptoms to those specified. For further advice and diagnosis, book an appointment at Sandhurst Urology.
How testicular cancer is diagnosed
Your GP will usually begin diagnosing testicular cancer with a physical exam. After asking about your symptoms, how long you have had them for, and whether other men in your family have had testicular cancer, your GP will feel the testicles to check for deformities.
If they suspect testicular cancer, your GP will request other tests to confirm it. These can include:
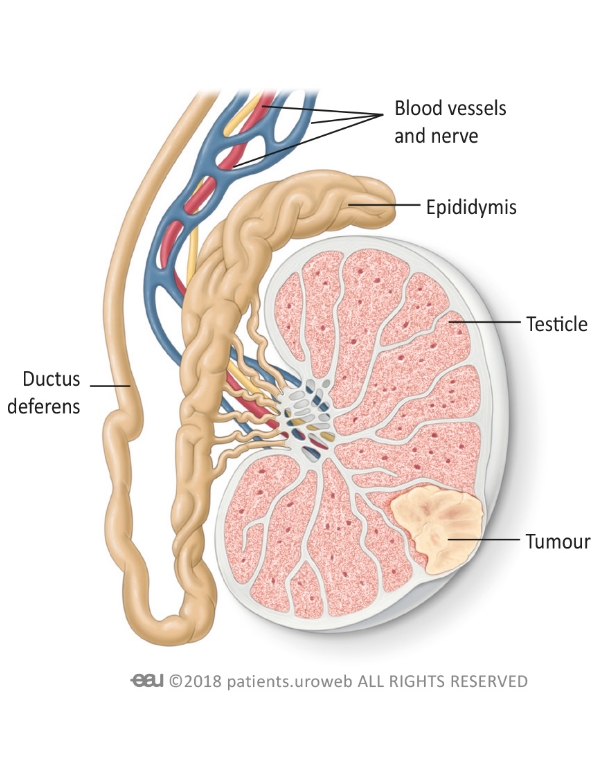
- Ultrasound – using sound waves to create an image of the testicles, this test lets your doctor identify abnormal size, shapes, or masses in the testes. It may show whether a tumour is present and how large it is.
- Blood tests – these check the levels of certain proteins in your blood, such as alpha-fetoprotein (AFP), beta human chorionic gonadotropin (beta-hCG), and lactate dehydrogenase (LDH). Abnormally high levels of one of these chemicals can indicate testicular cancer and help identify its type. As over-the-counter pregnancy tests check hGC levels, they may show positive results if you have testicular cancer; however, these should not be relied on for diagnosis.
- CT scans and MRI scans – though not typically used to diagnose primary testicular cancer, these tests may identify whether it has spread to other parts of the body. Your doctor may request one if your testicular cancer has been undiagnosed for some time, or if you have had testicular cancer in the past and it may have returned.
Preventing testicular cancer
There are currently no known causes of testicular cancer, and very few known methods of prevention. Current studies do not show a relationship between testicular cancer and lifestyle factors, such as diet, testicular injuries, strenuous activity, wearing tight clothing, or hot baths. However, the following strategies may help reduce your likelihood of developing it:
- Quit smoking – though there is no proven link between testicular cancer and smoking, smoking is a known cause of many other genitourinary and reproductive cancers. Avoiding tobacco consumption may lower your risk of developing testicular cancer
- Perform regular self-checks – the most effective way to catch testicular cancer in its early stages is by conducting regular self-examinations of the testicles, feeling for lumps, swelling, or abnormalities. Speak to your doctor if you notice any concerns.
- Practice safe sex – Some evidence suggests that men suffering from HIV/AIDS may have an increased risk of developing testicular cancer. Using barrier contraceptives such as condoms can prevent these diseases and therefore may reduce your testicular cancer risks.
Other non-preventable health conditions – such as male infertility, Down syndrome, or a history of undescended testicles after birth – may also contribute. If you suffer from any of these conditions, regular self-checks may particularly lower your testicular cancer risk.

Treatments for testicular cancer
Testicular cancer is highly curable, especially if it is identified early. Non-surgical treatment options for it can include:
- Radiation therapy – high dose x-rays targeted at the tumour can kill testicular cancer cells. Your doctor may recommend radiation therapy to treat the primary tumour itself, or to help prevent testicular cancer from returning after other treatments.
- Chemotherapy – these medications aim to kill testicular cancer cells or slow their growth while minimising damage to healthy cells. Chemotherapy may treat testicular cancer on its own, or may be recommended alongside other treatments such as surgery.
Medical interventions for testicular cancer
Treatments offered through Sandhurst Urology’s Bendigo clinic include:
- Orchidectomy – the most common treatment for testicular cancer, orchidectomy involves surgically removing the affected testicle and the tumour along with it. As removing the testicle can give the scrotum a deformed appearance, you may wish to have a prosthetic testicle placed to preserve aesthetics.
- Lymph node dissection – as the lymph nodes can store cancer cells, your surgeon may recommend removing them to help prevent testicular cancer from returning. This is a major surgery which may cause infertility and erectile dysfunction, so it is generally performed only if your surgeon believes it will significantly benefit your long-term health.
Providing Excellent Urological Care of the Highest Standards
Book a consultation with Sandhurst Urology today