Scrotal infections
What are scrotal infections?
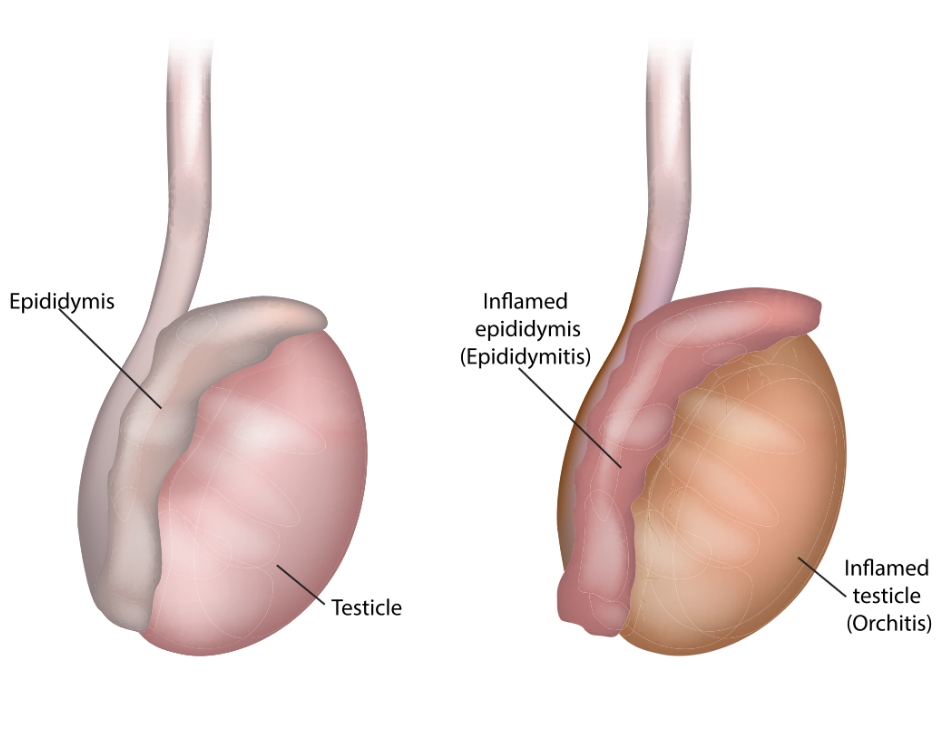
Scrotal infections are infections which affect the bag of skin that houses the testicles and lower parts of the spermatic cord. The scrotum houses many essential organs and structures which are vulnerable to infection – these include the epididymis, the tube at the back of the testicle which stores and carries sperm, and the testicles. These two structures sometimes fall vulnerable to infection at the same time (known as epididymo-orchitis).
Sandhurst Urology offers diagnosis, management, and medical intervention for scrotal infections from our clinic in Bendigo. To book an appointment, please ask your GP for a referral.
Symptoms of scrotal infections
Different organs within the scrotum can become infected, and the exact symptoms produced may vary depending on the infected structure. These symptoms may include:
- Tenderness and swelling in the scrotum
- Fever and chills
- The scrotum feeling abnormally warm to the touch
- Heaviness in the scrotum
- The scrotum or testicles feeling ‘tight’
- A feeling of pain or tightness in one or both testicles
- Intense pain inside the testicles
- Unusual discharge from the penis
- Blood in the urine or semen
- Pain or burning during urination
- Pain or burning in the groin region
Remember that your own experience with a scrotal infection is individual – you may not experience all the symptoms listed here, and you may experience others that are not listed. Seek professional advice from Sandhurst Urology to effectively diagnose and manage a scrotal infection.
Preventing scrotal infections
There are many steps you can take to reduce your risk of developing a scrotal infection. In addition to strategies recommended by your doctor, prevention methods may include:
- Practicing safe sex – using barrier contraceptives, such as condoms, can greatly decrease your chances of contracting STIS such as chlamydia or gonorrhoea which can cause epididymitis.
- Following post-surgical care recommendations – if you undergo a procedure on the testicles and/or scrotum, your doctor will instruct you on how and when to change dressings and clean the surgical site as you recover. Following these instructions helps prevent bacteria from entering the surgical wounds and causing an infection.
- Considering vaccinations – though data is limited, some studies show a correlation between developing a scrotal infection and having had the COVID-19 virus. Keeping up-to-date on vaccines and booster shots may help lower your risk.
How scrotal infections are diagnosed
Scrotal infections generally cannot be diagnosed through a physical exam alone. After asking about your symptoms and medical history, your doctor will generally recommend one or more tests to assess the infection’s severity and type. These tests, which can then inform a course of treatment, may include:
- Urinalysis – your doctor may ask you to provide a small sample of urine which is analysed for bacteria in a pathology lab. The test can help identify the type of infection you have, its extent, and which medications or procedures will best treat it.
- Urine culture – similar to urinalysis, a urine culture involves taking a sample of your urine and sending it to a pathology lab. Pathologists add growth-promoting substances to the sample which causes bacteria to multiply, making them easier to see and identify.
- STI checks – as sexually transmitted infections can cause scrotal infections, your doctor may recommend STI screening to identify any other diseases present.
- Ultrasound – your doctor may recommend this non-invasive imaging test to assess the soft structures and blood flow within the scrotum. The test may help identify other damage or causes of your symptoms.
Treatments for scrotal infections
Most scrotal infections are caused by bacteria and can be effectively managed through rest and medication. Treatments recommend by your urologist may include:
- Antibiotics – your doctor may prescribe medications which aim to kill the bacteria causing the infection. These may be taken by mouth (oral antibiotics), or come as a cream which needs to be applied to the infection site (topical antibiotics).
- Pain medication – over-the-counter anti-inflammatory medications such as Nurofen may be recommended to help ease pain.
- Rest and elevation – many men find that lying down with the scrotum elevated and periodically applying cold packs can relieve discomfort.
Medical interventions for scrotal infections
Scrotal infections can generally be managed through conservative treatments alone and rarely warrant surgical intervention. However, surgery is sometimes recommended to manage severe cases and prevent further damage. Sandhurst Urology provides surgical treatment for scrotal infections where needed, with options including:
- Aspiration – pus can often accumulate inside the scrotum, forming an abscess which requires surgical drainage.
- Epididymectomy and/or orchidectomy – in rare cases where testicles or epididymis become deeply infected, surgery may be required to remove them. This procedure is generally recommended only if the infection is severe and other treatments are unlikely to be effective.
Providing Excellent Urological Care of the Highest Standards
Book a consultation with Sandhurst Urology today