Retractile testis
What is a retractile testis?
A retractile testis is when one or both testicles are present in the scrotum at birth, but retreat back inside the abdomen later on. They are not to be confused with undescended testicles, which are testicles that are not present at birth and remain as such.
Testicles develop inside a child’s abdomen during pregnancy, before dropping or descending into the scrotum in the third trimester. They generally remain in the scrotum thereafter, though they can retract back into the abdomen under certain conditions (such as when a boy is cold). In some boys, the cremaster muscle which causes this retracts more than normal and one testicle remains inside the body for most of the time.
Sandhurst Urology offers diagnosis, management, and medical intervention for retractile testis from our clinic in Bendigo. To book an appointment, please ask your GP for a referral or call us directly.

Symptoms of retractile testis
The main symptom of retractile testis is an inability to feel one or both testicles inside the scrotum after they has previously been observed there. This is usually not painful, though it may give the scrotum an unusual appearance. Most parents notice it in their children while changing a nappy.
You or your child may be able to manually move the testicle back into the scrotum, and the testicle may remain in place for a time (if the cremaster muscle is fatigued). Though it may spontaneously retract and reappear again throughout childhood, it usually remains primarily in the scrotum by puberty.
Later in life, a retracted testicle may lead to fertility issues. As the testicles need to be 2-3 degrees lower than body temperature to produce sperm, testicles which remain inside the abdomen cannot mature effectively. This means that retractile testis may contribute to fertility issues.
Remember that your own experience with retractile testis is individual – you may not experience every symptom and may experience slightly different symptoms to those specified. For further advice and diagnosis, book an appointment at Sandhurst Urology.
How a retractile testis is diagnosed
Your doctor can diagnose retractile testes with a physical exam. While your child is sitting or lying down, the doctor will gently feel the scrotum to confirm that the testicle is present though not in its correct position. If they can feel the testicle, they may guide it back into position with their hands. A retractile testis generally remains in place after being manually relocated, at least temporarily.
If the doctor can feel the retracted testicle but cannot guide it into position or keep it there, the testicle may be diagnosed as ‘ascended’ or ‘acquired undescended’ instead. Ascended testicles may require surgery to correct.
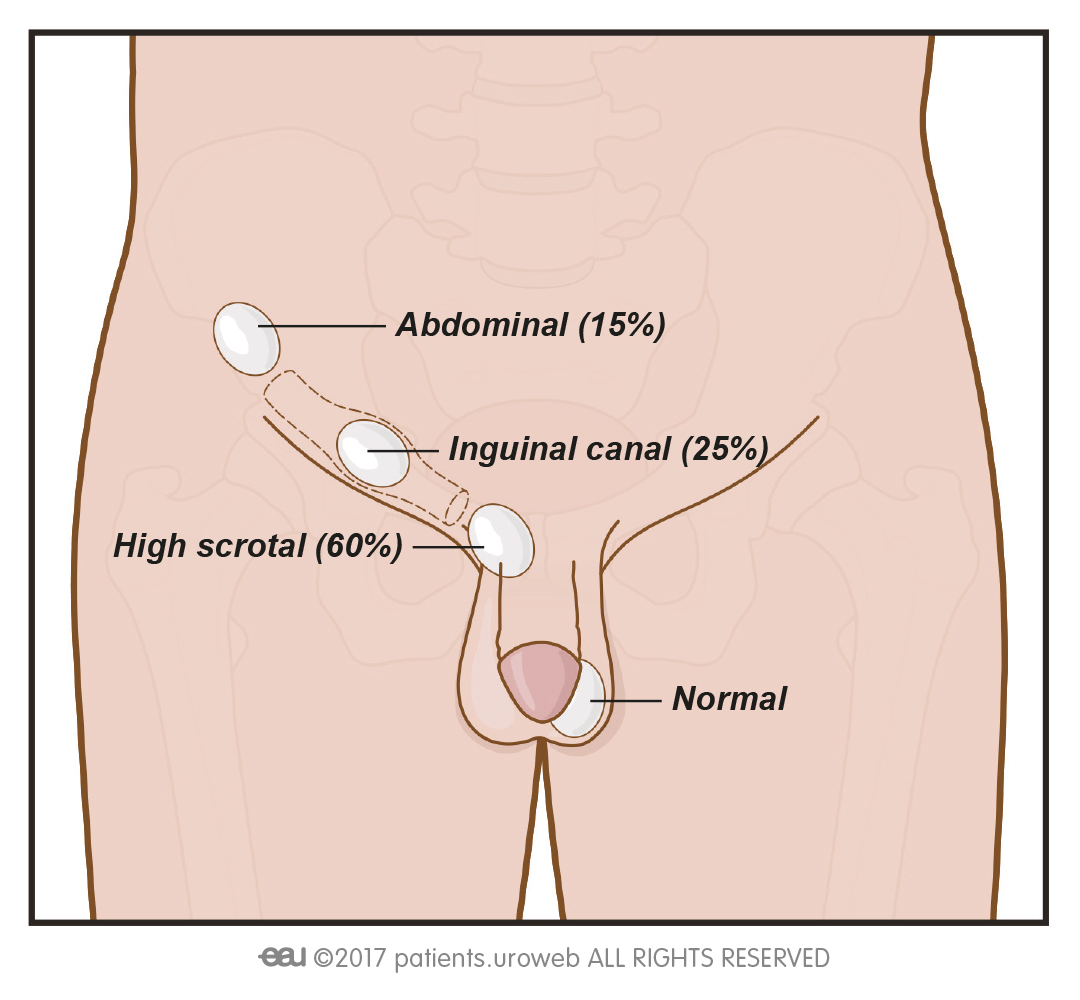
If the doctor cannot feel the testis or cannot guide it into the scrotum manually, they may recommend a laparoscopic surgery. This procedure involves the doctor using a small camera to look around inside the abdomen and determine whether the testicle is present – if present, the doctor may use specialized tools to attempt to relocate it and secure it in position. Since retracted testes are difficult to identify through ultrasound and other imaging methods, this is the most reliable way to diagnose them.
Preventing retractile testis
Little can be done to prevent retractile testis after birth, though some factors are known to influence its development while in utero. The following are factors which may increase a person’s risk of developing retractile testes; though they cannot be prevented outright, acknowledging and managing them effectively may help reduce the condition’s impact.
Treatments for retractile testis
Most cases of retractile testis resolve on their own before puberty, benefitting instead from being monitored as a boy grows. Methods used to do so may include:
- Observation – in many cases, the retracted testicle returns into the scrotum on its own and remains in place most of the time by the time a boy reaches puberty. Rather than acting immediately, your doctor may recommend regular check-ups (usually yearly) to monitor whether it descends on its own and act if it needs further corrective measures.
- Manual manipulation – after locating the testicle inside the abdomen, your doctor can gently guide it into the scrotum with their hands. This can usually be done in the same appointment as the initial diagnosis, though it may retreat into the abdomen again.
- Performing regular self-checks – men with retractile testis may have greater risks of developing testicular cancer and testicular torsion later in life, even if the condition is repaired or goes away. Your child may benefit from learning to check his own testicles from an early age.
Medical interventions for retractile testis
Surgery is usually recommended only if the testicle does not remain in the scrotum at least most of the time by puberty or if it does not descend at all (an ascending or acquired undescended testicle). If an ascended testicle does develop, surgical options for treating it include:
Orchidopexy – the surgeon separates the testicle and spermatic cord from any nearby tissues that may cause it to retract, then moves the testicle into the scrotum and stitches it into place. This is usually enough to keep the testicle in place, though some more complex cases may require a second procedure.
Laparoscopy – if the doctor cannot palpate the undescended testicle, they may recommend this procedure to determine whether it is present. Depending on the testicle’s condition, the doctor may use the same procedure to guide it into position or remove it (orchidectomy).
Providing Excellent Urological Care of the Highest Standards
Book a consultation with Sandhurst Urology today